Blown - Life after my ACL rupture - 2
 Sunday, April 22, 2018 at 02:23AM
Sunday, April 22, 2018 at 02:23AM  Better days with KarolIt’s been just over two weeks since my knee injury. The swelling is down and the range of motion is much better. I think I’ve arrested the rapid atrophy of my left quad. I gingerly stepped under my squat rack several days ago to see how things felt. I was already doing pistol box squats on my right leg but knew that getting the left back on line would help things going into surgery in another week or so. I typically squat to a box to ensure depth so for the current project I simply built the box height to a level that felt comfortable. As swelling has subsided and range improved, I’ve lowered the box height incrementally.
Better days with KarolIt’s been just over two weeks since my knee injury. The swelling is down and the range of motion is much better. I think I’ve arrested the rapid atrophy of my left quad. I gingerly stepped under my squat rack several days ago to see how things felt. I was already doing pistol box squats on my right leg but knew that getting the left back on line would help things going into surgery in another week or so. I typically squat to a box to ensure depth so for the current project I simply built the box height to a level that felt comfortable. As swelling has subsided and range improved, I’ve lowered the box height incrementally.
 Doing what I can to save my sanityThe most important thing to note with this increase in demand is that I’ve had no episodes of instability. This allows me to do things like this without feeling precarious or even injurious. Conversely, many patients with ACL disruptions feel their knee give out even with simple changes in direction, say, in the kitchen. Obviously, this would make something like barbell squatting out of the question. But for me, half squats feel fine and probably treat my aching brain and psyche as much as my neuromuscular system. I’ve worked up to 115 pounds now. I might add 10 or 20 more pounds before I fly out this weekend for surgery but likely nothing more than that. I’m doing between ten and twenty reps each set.
Doing what I can to save my sanityThe most important thing to note with this increase in demand is that I’ve had no episodes of instability. This allows me to do things like this without feeling precarious or even injurious. Conversely, many patients with ACL disruptions feel their knee give out even with simple changes in direction, say, in the kitchen. Obviously, this would make something like barbell squatting out of the question. But for me, half squats feel fine and probably treat my aching brain and psyche as much as my neuromuscular system. I’ve worked up to 115 pounds now. I might add 10 or 20 more pounds before I fly out this weekend for surgery but likely nothing more than that. I’m doing between ten and twenty reps each set.
There is a known neurological link between quadriceps function and ACL integrity. It likely represents a protective mechanism that keeps us from injuring our knee further after initial injury. This “circuit” is exceedingly variable from patient to patient. I’ve seen patients who have nearly a completely flaccid quad after injury and others who maintain decent muscle tone. The former is a bummer from a rehabilitation standpoint as it really slows the process. There’s simply no predicting it but you’re left with what you have and go from there. Electrical stimulation of the quad in the early post period can help bring things around in some patients.
So, that’s where I’m currently at. The waiting for surgery is a little difficult since I know that whatever recovery I’ve experienced is going to be nearly erased with the slice of the scalpel in a few days time. Set the clock to zero. But after that, it’s full speed ahead within the parameters of a sensible post-operative rehab plan. But before we get to that, there are some important considerations that need to be detailed and attended to. Over that last two and half decades of orthopedic work, one thing I’ve learned is that the average patient is completely under informed about what to worry about when it comes to “getting their knee fixed”. I’m here to help. Ignore these details at your own peril.
 Timing
Timing
You blew your knee. Now what? In the modern age, a big, fat, swollen and painful knee that got that way from an “event” needs proper medical evaluation. For me, this means a visit to a fellowship-trained orthopedic surgeon for a proper examination and a trip through the MRI scanner to slice through the fog of the injury and evaluate all the key structures. The list of potential diagnoses is relatively small but differentiating between them is vital to deciding what to do next. This should be done in the first few days since some injuries require much more care and immobilization that others. Don’t wait around for long if you can avoid it. The other concept of timing is when to have surgery, if indicated, and I’ll get to that in a bit.
Just to back up for a second, I want to be clear about choosing a surgeon. Having been in the business for a long time and had the pleasure of working with dozens of surgeons I can honestly say that you can “potentially” get good orthopedic care from nearly any trained orthopedist. Hell, some guys are good during their residency. But when it comes to me or my friends and family, I steer them to doctors who, 1. specialize, 2. have additional training in that specialty, and 3. are busy. Let’s break this down.
Choose your surgeon wisely
Depending upon the community in which you live, your options for orthopedic care can range from a generalist to a fellowship-trained, board-certified surgeon. The differences in training are not to be under estimated. A doctor can practice medicine of some sort right out of medical school, provided he or she passes the exit exams. The rare few that have opted out of the typical specialty residency that I’ve come across in my career (there have been one or two) end up as assistants to other physicians. Not common.
Most MD graduates apply to and go through some sort of residency program in the specialty of their choosing. These spots are competitive and not everyone gets what they want. These programs range in length depending upon the complexity of the specialty. Family practice, for instance, is many years SHORTER than, say, neurosurgery. The typical orthopedic residency is five years with the first year spent in general medicine training as the classic “intern”. From there, all training involves a wide range of orthopedic subspecialties. These include sports, total joint replacement, spine, foot and ankle, hand and upper extremity, tumor, pediatrics, trauma, etc. Any doctor who has completed a orthopedic residency has a wide level of experience that can lead to a viable orthopedic career. This is the generalist.
In this day and age, however, more ambitious orthopedic surgeons often chose to do additional training in one of those subspecialties. This is a fellowship. Most of these involve an additional year of intensive surgical training with a busy orthopedist that basically “hosts” the surgeon for the time. One or two surgeons each year are typical in these programs. Once again, fellowships are very competitive and are usually only offered to residents who demonstrate higher levels of skill. The value of this additional year of training should not be underestimated. The sheer volume of patients seen and cases performed hones the skill of surgeons who complete them.
In all fairness, a generalist who opts to specialize and builds a practice with that in mind can develop skills and judgement similar to a fellowship trained surgeon. On the other hand, those concepts will be his own rather than those of another surgeon who has been in practice a long time. I believe there is significant value in the latter. That’s just my opinion, of course.
With all this in mind, when you hurt your knee, go see someone who does a lot of knees and, as is my preference, has additional training in knee surgery. This is typically what is known as a “sports fellow”. In addition to finishing a sports fellowship, these surgeons will typically attempt the daunting process of board certification offered by the American Academy of Orthopedic Surgery. Unfortunately, not all fellows are brilliant surgeons so it’s still not a guarantee that you will get the best care. The truly diligent patient will dig down one more level and seek out others who might be able to direct them. I think one of the best resources is the local busy physical therapy practice. These guys see lots of patients from all surgeons in the community and see first hand who does well and who doesn’t. Ask around.
Be wary of the so-called “nice guy” surgeons. Just because you’d have a beer with them or you see them on the ski hill doesn’t mean they’re good in the operating room. To wit, one of the busiest surgeons I’ve ever worked around never skied. He was also weird and often an asshole. But the guy had chops where it mattered and likely did the lion’s share of ACLs in Jackson Hole over the years. He was also the man who coined the phrase…”there are two types of skiers in the world. Those that have blown their ACL and those that will.” I hated him for saying that but he’s more right than wrong.
 I know the feeling
I know the feeling
Timing - Early or Late
When to proceed with ACL reconstruction is a somewhat controversial topic. Opinions often vary regionally in the country. The recommendation from your surgeon will often hinge on his/her training and additionally on his/her experience. You basically have two choices and both have their merits and drawbacks. Let’s break it down.
Early
I’ve always maintained that your leg is never as fit as it is the moment you injure it. Everything is downhill from there. Swelling, inflammation, pain and muscle atrophy become big players right away. The longer you wait, the more entrenched some of these factors become. Having surgery soon after your injury avoids prolonged exposure to some of these concerns. Surgeons who live in ski towns are often big fans of just “getting it done”, often the day after the injury. Skeptics will say that the only reason for this is that patients are commonly tourists and the surgeon doesn’t want to let the business get away. Any problems the patient may have after the surgery will likely show once they go home so the surgeon is free from the burden of follow-up. Fair enough. Patients, on the other hand, believe that ski area surgeons are truly expert in treating the injury they’ve sustained. It’s hard to argue this point. Additionally, ski town surgeons make special concessions regarding scheduling in order to get the case done in short order. Patients going home to get their reconstruction will often have to get in line and start the process from scratch.
Injuries in addition to the torn ACL such as meniscus tears, medial or lateral collateral ligament injuries, posterior cruciate ligament ruptures (rare) or concomitant fracture can drive the decision for surgery one way or the other. The MRI can tease out all of these possibilities. A large “bucket handle” tear of the meniscus leading to a “locked” knee is often an indication for early intervention to avoid additional injury to the tissue and possibly miss an opportunity for primary repair rather than resection of this important structure.
Late
There is a large cohort of surgeons who believe that letting the knee “rest” and settle down before proceeding with surgery is the better road to take. Part of this is based on the belief that early surgery leads to a higher incidence of arthrofibrosis or knee stiffness after the fact. In truth, for motivated patients, the orthopedic literature doesn’t really support this contention. Both early and late surgical patients do well in terms of getting motion back.
Waiting 6 to 8 weeks for knee surgery often gives a patient a chance to see what life might be like with an ACL deficient knee. There is a small percentage of athletes that will compensate well enough to perform without the ligament. Athletes who are not involved in cutting sports are the best candidates for this path. The risk of attempting this route is that additional episodes of instability can lead to further meniscal or articular cartilage injury. This needs to be considered carefully.
One misconception that needs to be destroyed right here is that having your knee reconstructed does NOT necessarily prevent later arthritis. Stable, reconstructed knees often still go on to significant osteoarthritis years or decades later. The current thinking on this is that the initial injury changes the underlying structure and quality of the joint surface (cartilage) and increases the eventual degeneration that follows with time. The take home point here is that you get your knee fixed so you can trust it, NOT to prevent arthritis. Of course, avoiding additional instability can save your meniscal tissue which indirectly preserves your joint over time.
Graft Choice
So, you’ve found your surgeon and you’ve committed to a surgery date. Beyond simply deciding to undergo reconstruction in the first place, the next big decision is what kind of graft to use. There are several considerations that are flushed out in the literature that I’ll try to distill here.
Allograft vs Autograft
An allograft is a piece of tissue from a cadaver. Tissue banks provide material that is appropriate for ligament reconstruction. This option is particularly handy for recurrent and revision surgery when other tissue graft options have been exhausted. But for your first go, the use of allograft is more controversial, depending upon who you ask. First of all, historically, due to how the donor tissue was processed, failure rates were reportedly high. Modern tissue sterilization techniques seem to cause less degradation of the graft material and may end up having significantly lower failure rates, perhaps even similar to using your own tissue (autograft).
Advantages of using allograft include faster surgical time, no donor site morbidity, less post operative pain and it’s simply easier for the surgeon. Downsides to allograft are worth considering. The most important thing that drives return to sport after reconstruction (in addition to return of leg strength and coordination) is graft incorporation and healing. It’s well-documented in the literature that healing times are likely months faster with autograft vs allograft. Cadaver tissue simply takes longer to develop its own blood supply and become “part of you”. If the knee is stressed prior to full incorporation, graft failure rate goes up. You simply can’t rush biology but the phenomenon happens more quickly when using your own tissue. Allograft is often recommended in older (over 50 years) and lower demand patients. Some patients simply don’t want to give up their own tissue for reconstruction so allograft makes sense.
On the other hand, using your own tissue (autograft) is preferred for high demand and younger patients. Failure rates are lower and incorporation rates faster. There is no risk of disease transmission which still exists in cadaver tissue. The downside is that there is an additional procedure involved to harvest the graft. I’ll discuss the morbidity with these options below.
Autograft Options
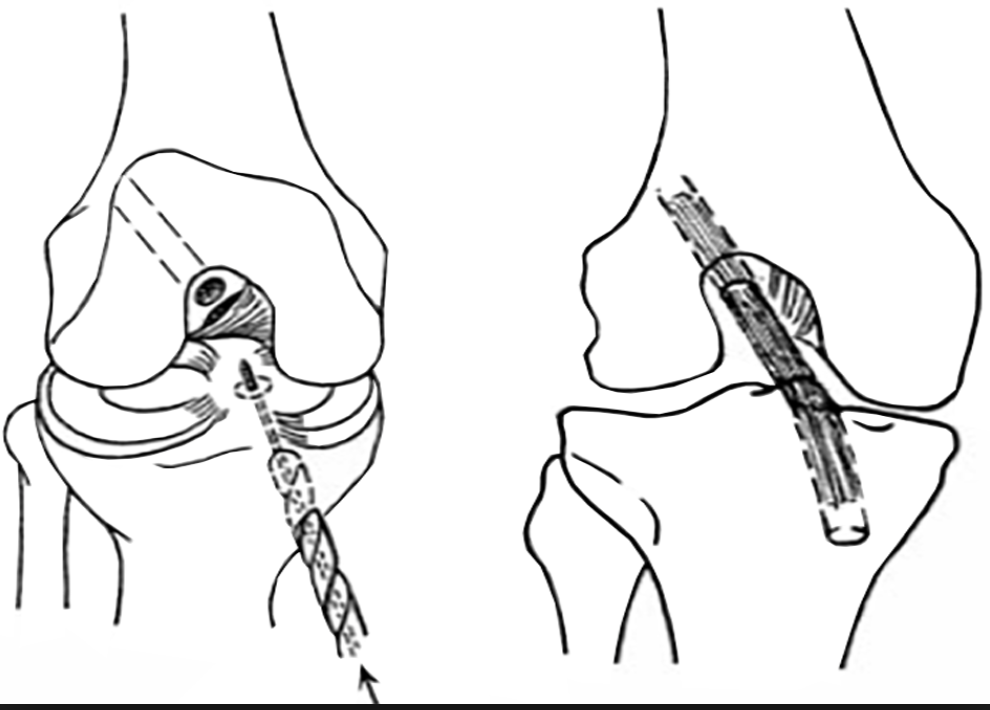
Patella bone-tendon bone
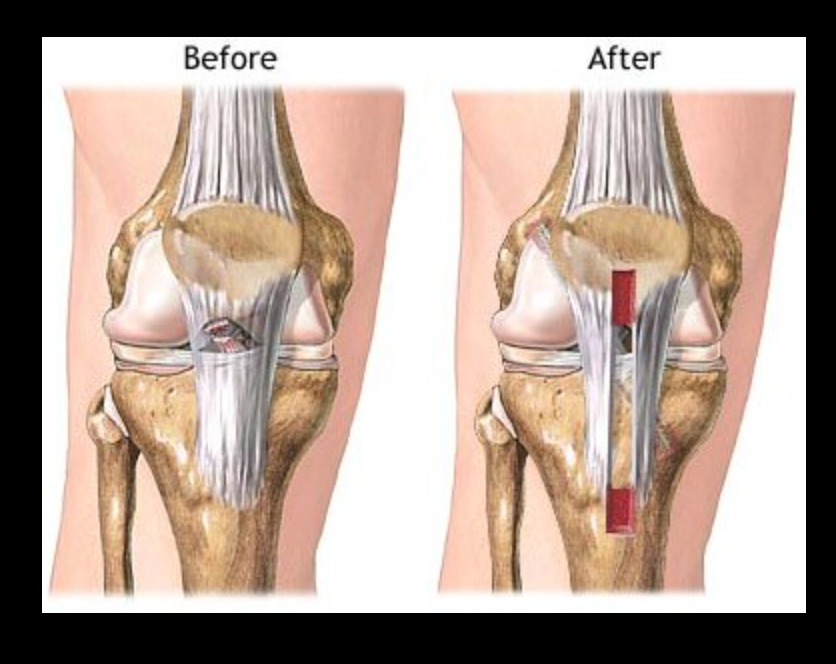
Considered by many to the the “gold standard” for ACL reconstruction, the patella BTB graft has a long history of success with high demand athletes. In my orthopedic training in the early 90’s, I did BTB exclusively with some of the most respected sports surgeons in the world. Advantages of this graft include a thick graft, bone plugs on both ends of the graft which heal inside the bone tunnels of the femur and tibia more readily and a high level of graft “stiffness” with a low rate of stretching out during recovery. The downside of BTB include donor site pain across the front of the knee, slow recovery times due to the same, long-term kneeling intolerance, some knee extensor weakness and possible early or late patella fracture from graft harvest.
Hamstring
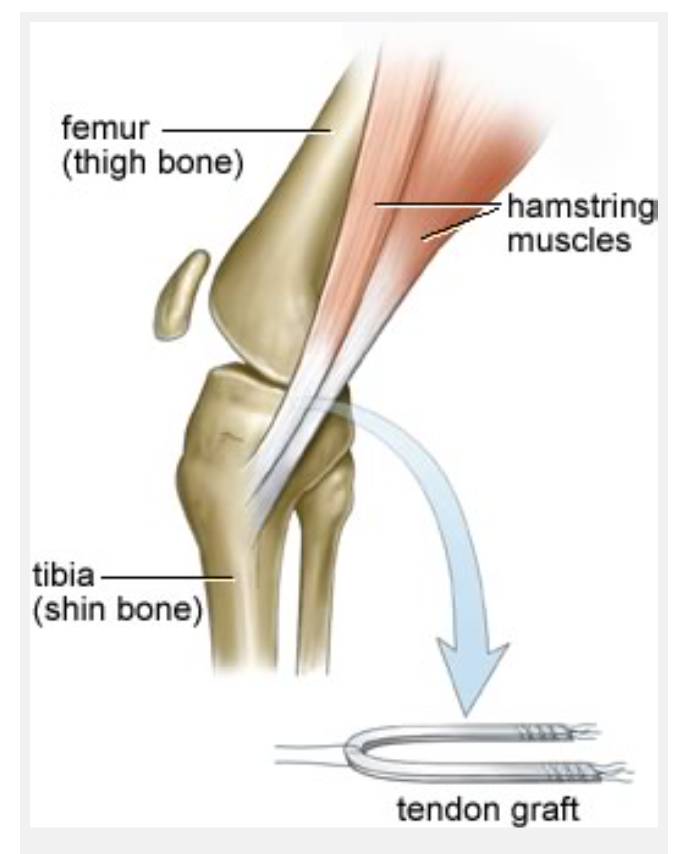
Semitendonosis and gracilis hamstring grafts have become the graft of choice for many high volume knee surgeons. The medial hamstring tendons are harvested through a small incision on the same side as the injury. The tendons are then braided or sewn together in an overlapped configuration that provides a ample graft for ACL reconstruction. Advantages include lower donor site morbidity, no knee extensor issues which facilitates more rapid range of motion return and no risk of patella fracture. Disadvantages include the absence of bone to bone fixation in the tunnels, sacrificing two medial hamstrings which can lead to minor knee flexor weakness and occasional increase in knee laxity after full healing. This latter issue is often unnoticed by the patient but is observable on exam.
Quadriceps tendon
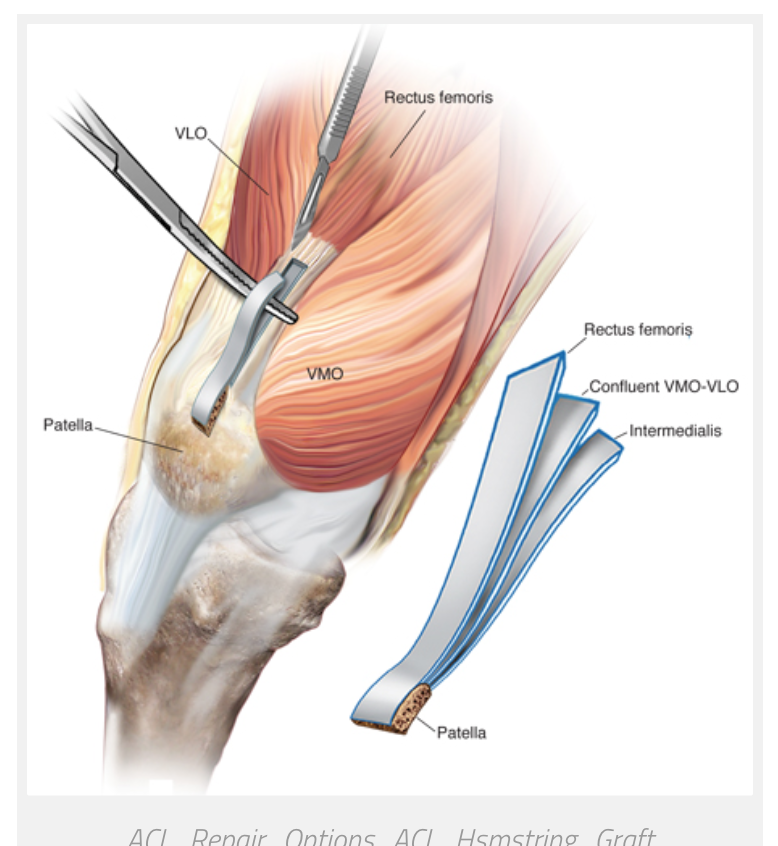
A less common but good choice of autograft is the quadriceps tendon from above the knee cap. This tendon is usually thick and harvesting typically leads to less anterior knee pain than the BTB described above. The option to take a bone plug from the upper pole of the patella is available at the discretion of the surgeon. Although I like this option conceptually, finding surgeons with long term experience with it is difficult.
Decision Time
Over the years, I’ve thought about what I would do should I ever need this procedure. I’ve helped surgeons perform hundreds of cases and seen mostly great outcomes with a variety of techniques. At 56 years of age, I would guess that most surgeons would default to a cadaver graft for my reconstruction and in fact, the surgeon who is performing my surgery admits to having never put autograft in someone my age. A theoretical argument can be made not to use my old ass tissue. Certainly, when it comes to cadaver graft material, the purveyors of the tissue do not use material from donors older than 40 years of age. The healing time is a significant consideration but so is the loss of my hamstrings. Am I willing to give up the bulk of next ski season, perhaps even all of it, to keep my hamstrings intact and have a easier time recovering from the surgery?
So, I’m going to have a cadaver allograft. It's hard for me to convey the conflict in my head about this decision. But the fact is, there are many surgeons around the world that put in almost exclusively allograft in all patients and have very high success rates. If I was thirty something, I might choose autograft. But I'm not. Monday the clock starts. Stay tuned.
 Brian |
Brian |  3 Comments |
3 Comments |  ACL reconstruction,
ACL reconstruction,  ACL rupture in
ACL rupture in  General
General 





Reader Comments (3)
Very interesting material. Thanks for the effort and good luck!
Thanks for reading and saying as much, Garrett.
Hi Brian,
Just a few words of encouragement from a fan of your site. With motivating not self-aggrandizing intent: I have now had ankle, knee, shoulder(spiral fracture of humerus plus broken collar bone and muscles partially detached from back right ribs-*80's SG crash) back-L4-L5 and two cancer surgeries. Plus I broke my hip in 3 places(though no surgery) due to bone density issues from that nasty oxaliplatin...
I have been as patient as I can with my body during recoveries, especially with chemo.
I'm still going "hard" enough in the mountains to have partners 15-20 years younger(I'm 50)..Although, I tend to recover waaaaay less quickly than them. Go slow(at first), be patient, Listen to your body, and you will be linking multiple 9k plus days before you know it.
Thanks for your blog,
Ollas